PHOTO
CAMBRIDGE – On May 14, 1962, the agriculture commissioner of Montana, Lowell Purdy, launched what would become one of the century’s great platitudes. “If we can put a man on the Moon,” he declared, seven years before the United States achieved President John F. Kennedy’s goal, “we surely are capable of seeing that our temporary surplus agricultural products are placed in many hungry stomachs of the world.”
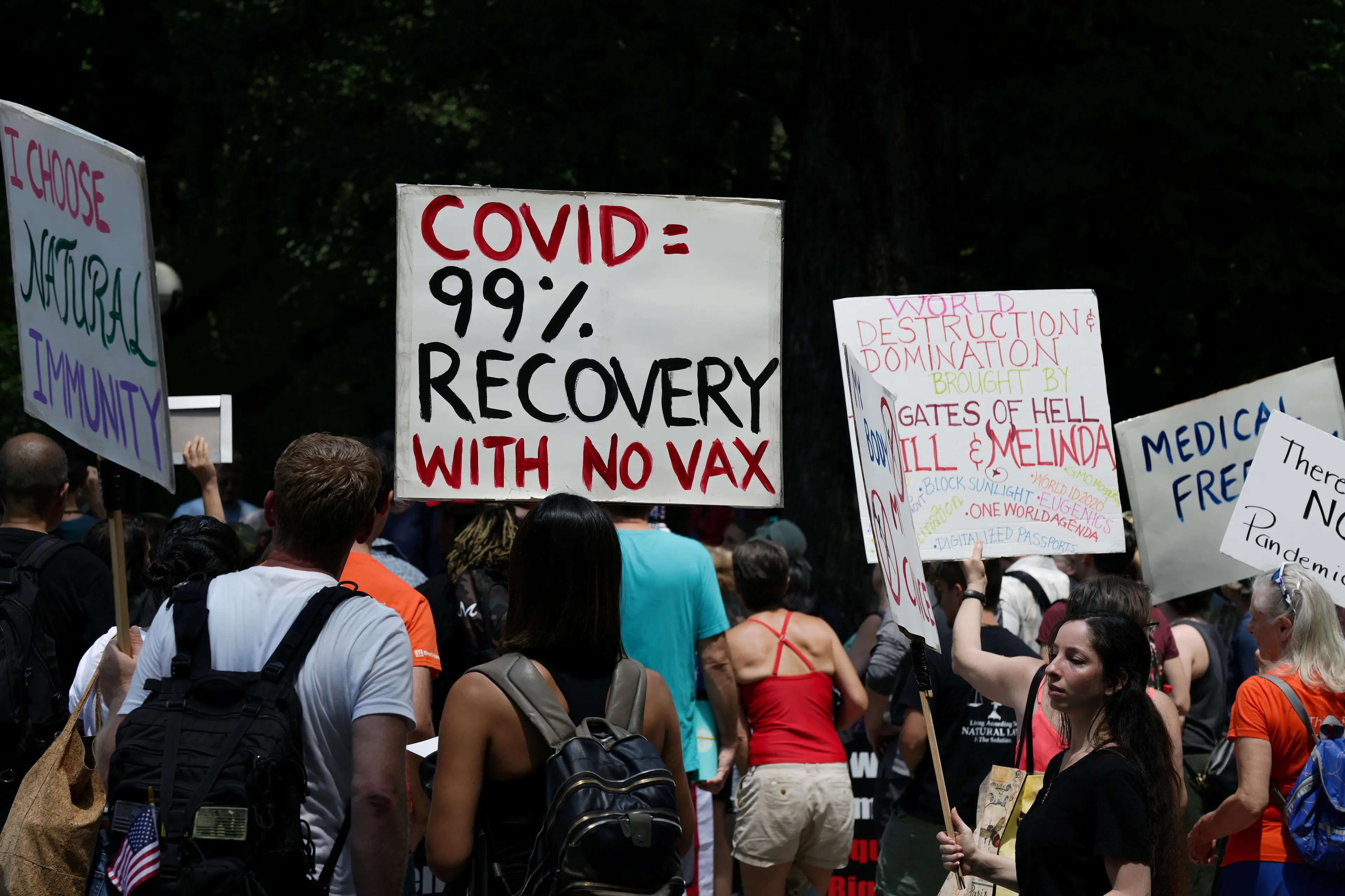
Since then, the formula has become a cliché – precisely because it often makes a pretty good point. Today, for example, one might point out: “If we can produce vaccines that drastically decrease the transmission and severity of COVID-19, we surely are capable of ending the pandemic.” And yet, we have so far been unable to do so, largely because people simply refuse to be vaccinated.
To be sure, in some cases – especially in lower-income countries – the primary impediment to large-scale immunization is limited vaccine availability. But in a country like the US, the main problem is vaccine hesitancy, even hostility. Although the Food and Drug Administration has granted emergency approval to three vaccines – a process that demands rigorous testing – many are convinced they are still “experimental,” and thus unsafe.
As Anthony Fauci, the head of the National Institute of Allergy and Infectious Diseases at the US National Institutes of Health, put it, there are two Americas, and their perceptions regarding vaccination are separated by a wall. For the America that mistrusts vaccines, the expertise of remote authorities and the logic of the scientific method are unconvincing.
Perhaps more tangible, real-world evidence can change their minds. It is certainly piling up: recent data show a strong negative correlation between vaccination rates and rates of infection, hospitalization, or death from COVID-19 across the US. In the week that ended on June 22, counties where 30% or fewer residents had been vaccinated suffered 5.6 new COVID cases per 100,000 people, whereas counties where more than 60% of residents had been vaccinated experienced just 2.1 new cases per 100,000.
On updated data, a one percentage-point increase in the share of adults (and teenagers) who were fully vaccinated in a given county as of June 9 was associated with a significant decline in the COVID-19 death rate – 0.06 per 100,000 inhabitants – over the subsequent 30 days (to July 9). That represents 2% of the total monthly coronavirus-related deaths. One could extrapolate from this that the statistical effect of reaching 100% vaccination would be to bring COVID-related deaths close to zero.
But, of course, correlation does not prove causality. The apparent beneficial effect of vaccination could, one might argue, be the result of some third factor, such as poverty. Low-income people are at higher risk of becoming infected with and dying from COVID-19, owing to a range of factors, from housing conditions to types of employment. If they are also less likely to get vaccinated, it could create the illusion that lack of immunization is the problem. Yet the beauty of econometrics is that one can control for third factors, such as the poverty rate or local temperature, to isolate statistically the effect of vaccination rates.
But this does not fully resolve the causality question. There is also the possibility that the simple observed correlation between vaccination and mortality understates the true impact of the vaccines. After all, those living in a high-risk context – say, near a transport hub – are more likely to know people who have suffered from the coronavirus, and thus might be more likely to get vaccinated. This “reverse causality” could lead to an apparent – and excessive – positive correlation between vaccination and death rates.
And, in fact, this could partly explain why earlier studies, conducted as recently as the beginning of June, did not find a clear negative correlation. But, as the highly contagious Delta variant gains traction among the unvaccinated, the correlation between immunization and lower COVID-19 infection and death rates is strengthening.
Still, to have a chance of convincing the vaccine skeptics, it is vital to disentangle causality from correlation. The key is to look at variations in vaccination rates that have nothing to do with where and how the coronavirus spreads – indeed, have nothing to do with the coronavirus at all. In technical parlance, we need an “exogenous instrument.”
Party affiliation or voting patterns are an obvious choice. Throughout the pandemic, Republican governors have been less likely than their Democratic counterparts to support public-health measures, such as mask mandates. Not surprisingly, Republican voters (45%) are less likely than independents (58%) and Democrats (73%) to accept vaccines. In counties where then-President Donald Trump won by a margin of 50 percentage points or more in the 2020 election, the vaccination rate was below 25%, as of April 17.
The “partisan gap” – which continues to widen – holds even after accounting for income, race, and age, as well as population density and the local infection and death rates. According to my calculations, when controlling for the poverty rate and other relevant variables (particularly age and temperature), a one percentage-point increase in the share of a county’s residents over age 12 who were fully vaccinated as of June 9 is associated with a death rate that was 0.05 lower per 100,000 inhabitants during the subsequent 30 days.
To ensure that the results are not distorted by reverse causality, I also performed another calculation, based on the same data. Accounting for variation in the vaccination decision attributable solely to partisan political affinity – and controlling for variables like poverty – I found the difference in the COVID-19 death rate to be 0.04 per 100,000 inhabitants.
I used voting patterns not to target any particular group, but rather to provide a better estimate of vaccine effectiveness on anyone. But I hope that at least some skeptics notice that members of their political “in-group” are dying at a higher rate, and decide to give vaccination a chance. As Rochelle Walensky, the director of the US Centers for Disease Control and Prevention, recently observed, “This is becoming a pandemic of the unvaccinated.”
Jeffrey Frankel is Professor of Capital Formation and Growth at Harvard University.
© Project Syndicate 2021
Disclaimer: The content of this article is syndicated or provided to this website from an external third party provider. We are not responsible for, and do not control, such external websites, entities, applications or media publishers. The body of the text is provided on an “as is” and “as available” basis and has not been edited in any way. Neither we nor our affiliates guarantee the accuracy of or endorse the views or opinions expressed in this article. Read our full disclaimer policy here.